- Temporary cardiac pacing
Temporary cardiac pacing
It is a therapeutic method used to treat acute conditions in patients with a slow heart rate, where the heart is unable to provide nutrients to all organs and tissues. In these cases, it is necessary to ensure a sufficient heart rate by means of electrical impulses that induce cardiac contractions - via a stimulating electrode inserted into the right ventricle of the heart.
A temporary electrode is left in the heart and the stimulation is switched on until the heart's own sufficient heart rate is restored. The temporary pacemaker is carried by the patient, usually attached to the arm. Due to the sensitivity of the pacing electrode to elevation with the risk of subsequent pacing failure, manipulation of the pacing system should be avoided. Changes of position should therefore preferably be performed with the assistance of a nurse. If the slow heart rate persists, a permanent pacemaker is implanted during the hospital stay or at a time that takes into account any associated diseases.
The insertion procedure is the same as for a permanent pacemaker, see permanent pacing.
- Permanent pacing.
Permanent pacemaker insertion
Cardiac pacing is indicated when the heart is too slow.
There are many reasons why the natural and regular rhythm of the heart is disturbed (e.g. myocardial heart attack, inflammation, etc.), or age-induced changes.
If the heart rhythm is too slow, and the body is also exposed to stress or strain, there are these symptoms:
- Vertigo,
- nausea,
- weakness,
- or short-term consciousness disturbance.
It is a sign that the heart is unable to perform its basic function – to supply enough blood to all the organs of the body – especially the brain.
The pacemaker function
The pacemaker delivers small, precisely timed electrical impulses to the heart muscle, causing the heart to contract regularly, just like a healthy heart. Today's modern pacemakers only work when the heart's natural rhythm is absent (i.e. they only work when needed). Therefore, the device must also be able to detect the heart's own rhythm, and if no spontaneous contraction occurs, the pacemaker will give a small electrical impulse to artificially induce this contraction by stimulating the heart muscle.
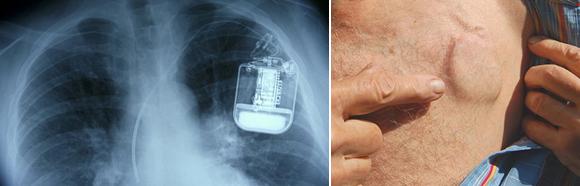
Pacemaker parts
The pacemaker consists of a battery and tiny electrical circuits, and its electrical impulses are transmitted through an electrode (which is a thin, full-length insulated wire) to the heart.
Pacemaker insertion
The procedure usually takes around half an hour. It is performed under local anaesthesia in the area below the collarbone. The position of the electrodes is checked on the X-ray screen. Once the electrodes have been tested, the pacemaker is attached, everything is checked again and the device is placed in a pre-formed pocket in the subcutaneous tissue and the pocket is sewn up with a few stitches. The procedure is painless.
Preparation before the procedure
Pacemaker insertion is performed while the patient is hospitalized in the cardiology department. The patient arrives the day before the hospitalisation, so the immediate preparation is done during the hospitalisation. It includes:
- Antibiotic prophylaxis (prevention of infection),
- shaving of the chest and underarms,
- insertion of an intravenous cannula,
- the patient is hungry from midnight (no food, drink, smoking),
- morning medication is administered, the patient drinks a small sip of water (tea).
Immediate post-operative care
- Stay hungry for two hours after the procedure.
- Stay in bed until morning. A drain is brought out of the wound, which the nurses check and record the amount of fluid in it.
- During the first few days after implantation, do not put up your hand on the side where the pacemaker is implanted, above the shoulder level and do not make any sudden movements with your arm or shoulder.
- After about a week, you'll come in to have the stitches removed.
The doctor must be informed in case of: (even after the hospitalization is over!!)
- Local symptoms – the wound area is still sore, abnormally red, warm, swollen or oozing fluid.
- General symptoms – fever, chest pain or twitching, prolonged fatigue, shortness of breath or worsening of existing shortness of breath.
Prior to discharge from the hospital, the patient will be scheduled for an initial outpatient check-up. No surgery will be its part – the check-up is painless. The function of the pacemaker, battery status and basic parameters of the device will be checked. Each patient is given a pacemaker patient card to carry at all times. It is also necessary to attend regular check-ups of the pacemaker.
Life with a pacemaker
You can safely engage in everyday activities (cleaning, showering, swimming, driving a car, after consulting a doctor you can resume physical activity (sports, hiking, gardening), hobbies, sexual activity. If you are not sure that your activity will affect the function of your pacemaker, always consult a medical professional.
Pacemaker and electrical devices
Common electrical appliances should not affect the function of the pacemaker. However, if you experience any unpleasant sensations (dizziness, fast or slow heartbeat) when using an electrical device, turn it off immediately or leave the area where it is located.
Feel free to use these devices
Radio, HI-FI, video, el. hair dryers, dryers, dishwashers, vacuum cleaners, microwave ovens, kitchen appliances, office appliances - fax machines, computers, telephones. It is better to put the mobile phone on the opposite side to the pacemaker and not to carry it in the breast pocket.
Be sure to consult your doctor in case of:
- Working with heavy vibrating equipment e.g. jackhammer.
- Using firearms.
- Working or staying near equipment with strong electromagnetic fields or high voltage.
- Using an electric welder.
Travelling
If you are travelling by plane, please inform security about the pacemaker or present your pacemaker patient card. The service will ensure that the check-in is safe for you. Driving a motor vehicle is safe. Always wear your seatbelt - it does not harm the pacemaker.
Medical check-ups and interventions
Before any check-up or intervention, alert the doctor to the implanted pacemaker. This applies to dentists, massage therapists and rehabilitation workers. Ultrasound, echocardiography and dental drilling are perfectly safe. In the case of special examinations - e.g. lithotripsy, radiotherapy, nuclear magnetic resonance (NMR) or electrocautery - your cardiologist should be consulted.
- Heart echo
Heart echo (echocardiography)
It is a painless and patient-friendly examination of the heart. No special prior preparation is required. The patient can eat, drink and take medication normally. It is performed by ultrasound. Ultrasound is nowadays the basic and probably the most widely used diagnostic imaging method. Its advantages are that it does not burden the body with penetrating radiation, it is not necessary to administer a contrast agent before the examination as with some X-ray methods, and it can, if necessary, be examined directly at the patient's bedside. Echocardiography allows the doctor to determine in a relatively short time how your heart is working and whether the heart valves are in good condition. It is also possible to observe your heart in motion.
The aim of the check-up is to determine not only the location, shape and size of the heart, but also to assess its structure, blood supply and, to some extent, cardiac function.
When is this examination performed?
When suspected of a disease in the areas of the heart muscle, heart intramuscular, valves and pericardium. Examination may reveal, for example, fluid in the pericardium, congenital developmental defects, infectious valve disease and heart tumours.
A valuable assistant to the doctor is the so-called. Doppler scanto map the blood flow through the heart cavities (atria and ventricles) to illustrate the narrowing or loosening of the valves and to calculate the blood pressures at different heart points.
This examination can be performed in the cardiology examination room or in the inpatient ward at the patient's bedside.
The patient is positioned on the back with the chest exposed. The doctor will apply a conductive gel to the end of the probe. He then passes the probe over the chest at different angles. The images of the heart are recorded and displayed on a screen. During the examination, the doctor will ask you to turn on your side. In total, this examination usually takes about 15 minutes.
After the examination no special regimen is necessary. You can eat, drink, take your medication and carry out your normal daily activities.
Your doctor will tell you the result immediately after the examination.
- Electric cardioversion
Electric cardioversion
Electrical cardioversion is a procedure used to stop heart arrhythmias, most commonly atrial fibrillation or flutter. These arrhythmias usually impair the heart's performance and can also lead to clots in the heart's compartments (atria).
This procedure is performed on an outpatient basis, i.e. without the need for further hospitalisation.
In cardioversion, a discharge of current is applied to the heart through the surface of the chest using a defibrillator to interrupt the arrhythmia and restore the heart's normal rhythm. To eliminate the pain perception during the discharge, cardioversion is performed while the patient is briefly sedated. Because of the need to monitor basic vital signs (breathing, blood pressure, heart rhythm), the procedure takes place in a specially equipped room (cardiac ICU room).
Prior to cardioversion
- Eat or drink nothing since midnight.
- Unless your doctor tells you otherwise, continue to take all medications on the day of the procedure (with a small amount of water).
- Expect to be supervised for 2 hours after the procedure.
- After this performance, you will not be able to drive the car until the evening.
Examination process
- A cannula will be inserted into a vein in your forearm, into which a short-term anaesthetic will be administered and medication as prescribed by your doctor.
- Adhesive electrodes will be placed on your chest to read the ECG waveform.
- Your blood pressure will be measured at regular intervals using an arm band.
- Medication will then be given to induce a short-term (a few minutes) deep sleep to remove the perception of pain.
- After you have been put to sleep, 2 defibrillator electrodes are placed on your chest and an electric shock is applied in a fraction of a second. If normal heart rhythm is not restored, the shock can be repeated immediately using higher energy.
- You will not feel the electric discharge, you may feel a slight weakness after the procedure.
- For 2 hours we will continue to monitor your vital signs (breathing, blood pressure, heart rate) and gradually we wake you up from your artificially induced sleep. During these 2 hours, you must not eat or drink anything.
After the procedure
You may feel soreness in your chest or back after the procedure. More often, you may feel a slight burning sensation on the surface of your body where the defibrillator electrodes were attached. These areas are usually red. In such cases, they are treated with ointment or burn cream.
During the 24 hours after the procedure, you should not drive motor vehicles or heavy machinery and drink alcohol. You should also take into account that your ability to concentrate or make decisions may be partially impaired and not leave serious decisions or signing of legal documents for this period.
After the procedure, you will be given a follow-up appointment with your cardiologist.
- Ergometry
Ergometry
Ergometry is an examination method that allows the doctor to monitor the work of your heart under strain. A bicycle ergometer is a device that consists of an exercise bike and an ECG measuring device. During the examination, the doctor studies the ECG curve and heart rate at different exercise intensities. The ECG curve and heart rate are sensed using electrodes attached to the chest and limbs.
The obtained ECG curves have a characteristic appearance, from which an experienced doctor can easily detect hidden heart disease. During exercise, changes may appear on the ECG curve that are not apparent on an ECG performed at rest while lying down.
The most common indication for this examination is to determine the nature of your heart disease (most often in diseases where the heart muscle is insufficiently supplied with nutrients and especially oxygen - IHD).
IHD (coronary artery disease) is a heart disease in which the arteries that feed the heart muscle become clogged with fatty particles. This condition leads to the formation of atherosclerotic plaques and a reduction in the diameter of the artery. Due to the reduced diameter of these arteries, the heart tissue is not sufficiently nourished and hurts. This disease is characterized by chest pain that increases with exertion when the heart requires a greater supply of oxygenated blood.
Based on this examination, the doctor then determines the severity of the disease.
Prior to examination
- Do not drink alcohol or smoke 12 hours before ergometry.
- It is possible to have a light meal before the examination.
- Take your temperature the morning before the exam. It shouldn't be elevated.
- Wear comfortable clothes and sports shoes to the examination.
Before the actual examination, the doctor will check you up and the nurse will record your ECG and take your blood pressure. If you do not feel well, tell the doctor at the start of the examination.
- HUT – Head-Up Tilt Test
HUT – Head-Up Tilt Test
The test is indicated to explore the cause of conditions characterised by sudden onset of unconsciousness associated with a fall, followed by a return of consciousness and correction of the general condition within a few minutes. The test is performed on a special electrically controlled tilt table with continuous monitoring of ECG, blood pressure and oxygenation of the body with oxygen. The whole examination takes about 45 minutes including patient preparation.
- In the first phase, the patient is calmed down in a horizontal position,
- in the second phase the patient is reclined to a position of about 60 degrees (feet down, head up) this phase lasts 30 minutes.
Preparation:
4 hours before the examination, do not eat or drink.
Contraindications:
- pregnancy,
- epilepsy,
- age - the examination is carried out up to the age of 70.
If required, the tilt can be immediately returned to its original horizontal position. During tilting, the human physiologically engages certain regulatory mechanisms that lead to a standard cardiac response in order to maintain blood pressure and circulation.
In certain cases, these mechanisms are disturbed, which is manifested by a significant blood-pressure drop, slowing of the heartbeat or, on the contrary, an abnormal increase in heart rate or arrhythmias. Difficulties are manifested by sweating, nausea, dizziness or a feeling of dryness in the mouth. All these manifestations are recorded and documented. Depending on the mechanism of the disorder of consciousness, treatment is then recommended by the physician.
- Telemetry
Telemetry
It is used to monitor the patient's heart rate, pulse rate and respirations remotely. The patient has this device attached to the chest with four adhesive electrodes. The patient's movement around the ward is not restricted, but the range is only within the cardiology ward. The tracking monitor is located in the nurse's station, so if the telemeter detects any irregularity in the patient's heart rhythm, it immediately sounds an alarm and the patient is given timely assistance.
- Coronary angiography
Coronary angiography (performed by KC Vysočina)
Coronarography is a contrast-enhanced radiological examination of the coronary arteries that supply blood to your heart (or heart muscle). It is performed when a narrowing or blockage of these arteries is suspected. The cause is most often atherosclerotic involvement in coronary heart disease (CHD). This is mainly manifested by chest pain and often shortness of breath.
The aim of the coronary angiography is to show the coronary arteries, their translucency and thus reveal any narrowing or blockage. To restore blood flow through the "clogged" or narrowed arteries, depending on the findings and possibilities, catheterization angioplasty can be performed at the same time, or after assessment of the findings, cardiac surgery can be planned at the CKTCH Brno or in České Budějovice (coronary by-pass = bridging of an impassable coronary artery).
Pharmacological treatment is an integral part of the investigation and treatment of IHD (see article - ergometry). Early detection of critical narrowing of the coronary arteries and initiation of appropriate treatment can by the means of coronary angiography save a life.
It is also performed before any planned surgical procedure on the heart and its vessels.
The coronary angiography unit is a combination of an surgery room and an X-ray room. It includes a surgery table and an adjustable stand with an X-ray machine. A radiation source is required for X-ray imaging - the so-called X-ray machine. After passing through the body, the X-rays are scanned and transferred to a screen. Once the cross-section and course of your coronary arteries have been imaged, a contrast medium must be injected, which is done with a catheter inserted to the heart. This is a long, thin, hollow tube. The contrast medium is injected with a pressurised syringe.
The catheter is usually inserted into the artery through the wrist or also through the groin... Under X-ray control, the catheter is passed through your artery to the point where the coronary vessels are separated above the aortic valve. After entering the coronary artery, the doctor injects a contrast agent to show its translucency and course. The doctor repeats the same procedure for the other coronary artery.
Preparation:
- Long term – the indication for the examination is determined by the physician, the patient receives an appointment for the examination and presents to the hospital on the morning of the scheduled coronary angiography. Blood is sampled beforehand, mainly to check for clotting.
The patient arrives at the hospital hungry, but takes his morning medication as prescribed by his doctor.. Diabetics are an exception, they must not inject insulin or take diabetes medication !! They'll stay with an empty stomach!!
It is also necessary to report iodine and mesocaine allergies in time! - Short term
Shaving the forearm or groin.
Insertion of intravenous flexilla.
The cath lab then calls patients individually for the procedure. The nursing staff then take the patient in the bed for coronary angiography.
The process of examination
The patient lies down on the examination table under the movable arm of the X-ray. They can see the screen on the side, which the doctor will watch during the examination. The nurse will stick electrodes on the chest to read the ECG. You will be given a clip on your finger to read the blood oxygen saturation.
The doctor then disinfects the catheter insertion site (i.e. the groin or wrist) and numbs it with a small amount of local anaesthetic. Using a special needle, he or she will puncture the femoral artery and move the catheter upstream to the heart arteries and then inject the contrast agent. He will check the actual position of the catheter and the condition of your arteries by taking x-rays and watching a screen. The entire procedure is performed with only local anaesthesia at the catheter insertion site. You are therefore fully conscious and are always in touch with the doctor, who explains to you exactly what to do. All you have to do is to lie still on your back and occasionally hold your breath when prompted. The doctor can tell you the preliminary results of the examination during the examination. The procedure itself takes from 20 minutes to an hour.
During a coronary angiography, the doctor can perform a so-called PCI (=percutaneous coronary intervention) - this is a technique that can be used to dilate narrowed or closed blood vessels with a special balloon and very often a special spring in the artery, called a stent. The typical pinching pain behind the sternum is likely to occur after the balloon has been inflated. The balloon closes the artery for a while and oxygenated blood cannot flow into the artery.
During inflation, the sclerotic plaques are pushed against the vessel wall, thereby expanding the internal vascular permeability. The doctor then checks the patency of the blood vessel by re-inflating the balloon with a contrast agent and decides whether to re-inflate the balloon or to insert a stent (a tiny spring that leaves the blood vessel stretched).
How to make an appointment?
Tel: 567 157 156 or 567 157 157
How to prepare the patient?
- Long term – the indication for the examination is determined by the physician, the patient receives an appointment for the examination and presents to the hospital on the morning of the scheduled coronary angiography. Blood is sampled beforehand, mainly to check for clotting.
- Electrophysiological examination and catheter ablation
Electrophysiological examination (performed by KC Vysočina)
Electrophysiological testing is performed to diagnose a heart rhythm disorder (arrhythmia). This examination involves inserting catheters (special tubes) into the heart with the help of an X-ray machine. The catheters are typically inserted from the right groin. Common indications for this examination are palpitations (chest palpitations), syncope (sudden disturbances of consciousness) and some selected patients with heart failure to assess the need for an implantable device (ICD). Nowadays, in most cases, the diagnostic electrophysiological examination is followed in one session by the therapeutic part, i.e. catheter ablation, together with relieving the patient of his/her disorder.

Electrophysiological examination Catheter ablation is a method of treating some rhythm disorders. Ablation involves "burning" the area responsible for the arrhythmia by using catheters (tubes) to make heat at the location in the heart. Typically, catheters are inserted from the right groin or sometimes from both groins. In some cases, it is necessary to induce the arrhythmia so that the examining physician is able to determine where the arrhythmia is coming from. The success rate of catheter ablation is close to 100 % for some arrhythmias (e.g. ablation of flutter or regular supraventricular tachycardia), while for others it is lower and may be between 70 and 80 % (e.g. paroxysmal atrial fibrillation) or even below 50 % (e.g. persistent atrial fibrillation).
Examination and treatment with the catheter ablation requires the patient's cooperation, i.e. the ability to lie flat on the back for 1-3 hours in the operating room and then 8-12 hours in the inpatient ward. Catheter ablation is performed under analgosedation, i.e. after administration of strong analgesics, and can be uncomfortable at certain parts of the procedure. In our highly experienced department, catheter ablation is considered a safe treatment and is preferred to pharmacological treatment (drugs) in many indications.
The most common arrhythmia for which catheter ablation is currently performed is atrial fibrillation (irregular beats originating from the atria). This rhythm disorder, if untreated, carries an increased risk of hospital admissions, stroke and heart failure. The principle of atrial fibrillation ablation is to insert a catheter through the groin into the left atrium of the heart, where a series of "burns" are used to create circular lesions around the pulmonary veins that drain into the left atrium. Atrial fibrillation ablation is a technologically demanding procedure that uses modern navigation and computer systems. Typically, patients undergo a CT scan of the heart (computed tomography scan) a week before the ablation, and some patients undergo a complementary oesophageal ultrasound before the procedure. After ablation, patients are then left on or newly set up on anticoagulation therapy (e.g. Warfarin, Pradaxa, Eliquis, etc.) for a minimum of 3 months.
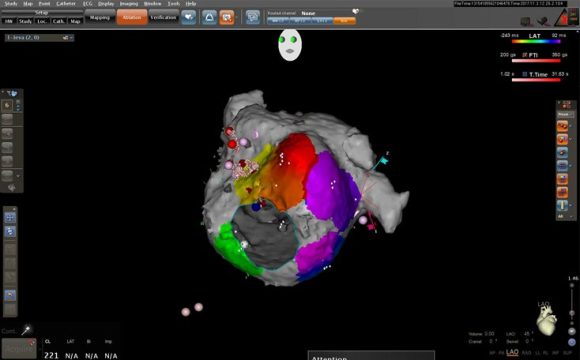
Navigation system used in the treatment of atrial fibrillation Implantation of an ICD (implantable cardioverter defibrillator) involves inserting an electrode (lead) from the left (rarely right) subclavian area into the heart and connecting it to a generator (power source) that is "sewn" into the subcutaneous tissue. An ICD is indicated for patients who are at risk of severe life-threatening arrhythmias, typically patients with heart failure. The defibrillator is able to detect these arrhythmias and treat them with either a series of rapid pulses or a strong electrical discharge. In about a third of patients, a special electrode is then indicated to be inserted into the vein surrounding the left ventricle to help them with the symptoms of heart failure (i.e. to improve breathlessness and reduce swelling of the limbs). The implantation of an ICD is similar in principle to the insertion of a permanent pacemaker, but in the case of an ICD it is slightly more robust and has a slightly shorter lifetime.

ICD (implantable cardioverter defibrillator) 
ICD (implantable cardioverter defibrillator) How to make an appointment?
Tel: 567 157 245
Cardiology Department